Communication is about more than just words—it’s tone of voice, body language, and facial expressions. Cadence, eye contact, gestures, body angles, and weight placement all have implications, which change depending on the social situation, the cultural background of speaker, and the status of the participants. As an actor whose specialty is Physical Theatre, and also as a person with a keen interest in interaction, empowerment, and culture, I have given a great deal of my life’s attention to these non-verbal cues.
Along those lines, I have taught workshops with some wonderful college students who are going into health-related fields, and who want to learn how to be better at reading a patient, and giving them the focus and attention they need most. I share with you some primary ideas, in hopes that they will be another way of looking at a moment, and perhaps useful.
Unpacking the situation
Status
Yours, theirs, the situation’s. Social Status and ‘Playing Status’
What is it? What do we mean? What is the most utilitarian understanding? (macro & micro)
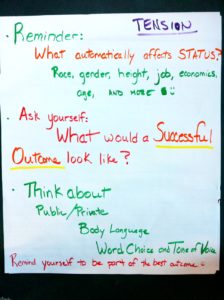
Using status to make the situation go well by making small adjustments and watching what the other people are doing; being aware of the impact your status has.
Fun performance exercise about status
- Reflection-what did we notice? Seeing it, using it, understanding it exercises.
- Why is it important?
- Care-giver and client
- Client and client
- Care-giver and care-giver
Subtext
What is it? What’s really being said even unintentionally. Remember: intention and reception are NOT the same—arms crossed over chest reads as “I’m not receptive,” even if all you feel is “I am cold!”
- Seeing it in action
- Unpack and relive
- Body Language
- Vocal Stuff
First 30-40 Seconds
First part of diagnosing (even in a non-health situation!) is in the first 30 seconds: How does the person feel about being there now? Are they ready to talk about condition or a treatment plan? Look for the body clues for stress, anxiety, and resistance to find a way to address these first. No matter WHAT field you are in, a successful outcome requires addressing these conditions first. Find a way to “yes” the emotional experience, even if you need to “no” a current practice or habit as part of your treatment plan.
Understanding by design
What does a successful outcome look like? What does well-being look like?
Conflict resolutions
- long term/short term
- private vs public
- strategic moment, hearable, impactful outcome
- understanding the importance of client resistance
Body Language
Reading Others: Look for tension, weight positioning, open/closed body language.
Making Choices: Most importantly, attend. Believe in the value of the other person, even if you disagree with their choices—it will increase your chances of success. Remember, a strong, established status through body language means your words do not need to be as forceful. Also, use the least amount needed; too much makes you threatening.
- Hold your head still when you speak
- Relax (add and release tightness/tension as needed)…especially your core, and try to breathe evenly
- Smooth, not fluttery movement
- No extra movements or word bits—better to be silent for a second than have ums, ers, and uhs
- Eye contact—direct without challenging, when to look away
- “Male” and “Female” head angles (right angles vs. tilt)
- Use of space and of objects in that space
- Point your open heart to the client!
Verbal Language
Think About…..
- Opening ‘address’. Use of title (Mr., Miss, Ms. Mrs.)? Use of first or last name, or nickname? Use of a cultural modifier (Dude, bro, yo, sweetheart, etc)? How connected or detached are you? This is your opportunity to set the TONE and the RELATIONSHIP.
- Humor. Yes, no, mixed. What kind? NOTE: Humor must NOT devalue the seriousness of the incident.
- Breath, pace
- Avoid extra words, ums, and charged language (but you already knew that)
- Building in their success
- Holding your ground when all else fails. If you are in the position of greater status, do it as gently as possible
Cultural Norms
“Kiss Bow Shake Hands”; “Cultural Differences in Non-Verbal Communication; health screening for children and adolescents by the Vermont Department of Health” & more
Eye Contact, Physical Contact, Space, Vocals
Group practice/problem solving: common situations. Remember to look for creative solutions to similar outside of your field as well! (e.g. Early Childhood Education tips)